Morphine Allergy
Question# 809
Also, I have seen several patients allergic to morphine, have hydromorphone or Dilaudid on prescription, why is this?
Answer:
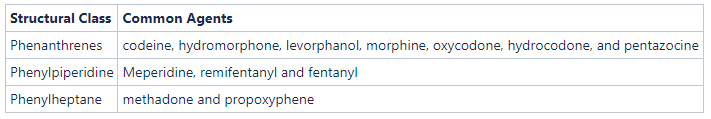
To answer your question specifically, for true IgE mediated allergic reactions, we would recommend choosing an opiate from a different medication structural class
Patients often report adverse effects after the administration of opiates. Common symptoms include drowsiness, dry mouth, and GI upset (N/V/constipation). Unfortunately, many of these patients will call this an “allergy”, a label that can follow them through the trajectory of their course of current and future treatment potentially leading to under treatment. Thankfully true reactions are rare, and published data suggests that as many as nine out of 10 patients labeled with an opioid allergy do not have a true allergy.
While these symptoms look like an allergy, they are technically and physiologically different. Pseudoallergy reactions result when direct stimulation of mast cells and basophils leads to the released of mediators such as histamine. Commonly, these are caused by low-potency opioids such as codeine, and generally produce milder symptoms (itching, flushing, sweating, mild hypotension, sneezing, etc.). A true IgE mediated, or T-cell mediated allergic reaction while extremely rare, may produce severe hypotension or cardiovascular collapse, angioedema, bronchospasm, cutaneous reactions, etc.
Psuedoallergies mimic true IgE immunologic reactions but are not immune-mediated.
Despite this, clinically these two reactions are indistinguishable, and we should err on the side of caution. Remember, that while most patients who say they are allergic to an opioid have experienced only a side effect that has been misclassified as an allergy
Therefore, in these patients, it’s important to choose a safe alternative drug. Patients should always be informed and educated about possible side effects of opioids and monitored for adverse side effects on a regular basis.
If you feel that the patient would truly benefit from opiate therapy, there are several strategies we recommend. Most importantly, use these medications low and slow, and practice using aliquots. Histamine release is dose-dependant, so use the lowest possible dose. Conversely, use a higher-potency opiate, which is less likely to cause histamine release.
We would also recommend choosing an opiate from a different medication structural class. Often, a patient who is allergic to an opioid from one class may be treated with an agent from another class without cross-sensitivity.
It’s also important to consider multi-modal analgesia and use non-opiate medications as well. Additionally, don’t forget the non-pharmacologic interventions as part of a robust analgesia bundle of care. All of these topics are covered in 2024 Spring CME.
For further information about allergies, we encourage you to check out the elective CME Critical Levels podcast about anaphylaxis, available on MedicLEARN.