CPR in Pediatric Bradycardia
Question# 939
My interpretation of this is that it stipulates paramedics need to follow the guidelines for CPR, regardless of the patient being VSA.
For example, in figure 12 of the Heart and Stroke Foundation Guidelines, for a pediatric bradicardia with pulse algorithm, paramedics should be following the guideline to initiate CPR if the heart rate is below 60bpm. This does not mean the patient is VSA, only that they are not perfusing properly and need us to assist them regardless of oxygen/ventilation administration.
I think this would need to be reviewed in CME. People seem confused about our responsibilities based on the Heart and Stroke Foundation
Answer:
You are correct that the BLS references the Heart and Stoke Foundation of Canada Guidelines with respect to initiating CPR. For definition’s sake, we will define a child a being 1 year of age until puberty (breast development in females and the presence of axillary hair in males). For those with signs of puberty and beyond, adult guidelines should be followed.
In that context, in the 2025 guidelines, the AHA has a Class 1 recommendation that “In infants and children with heart rate less than 60 beats/min and cardiopulmonary compromise despite effective ventilation with oxygen, start CPR”.
A class 1 recommendation is a strong recommendation that suggests the intervention benefit significantly outweighs the risk.
Their reasoning for this recommendation is that “bradycardia associated with cardiopulmonary compromise, even with a palpable pulse, may be a harbinger of impending pulseless cardiac arrest. As such, bradycardia with a heart rate of less than 60 beats per minute in infants and children should prompt an evaluation for cardiopulmonary compromise, including acutely altered mental status, hypotension or other signs of shock”. It’s about recognizing cardiopulmonary compromise early, not just waiting for a full arrest.
This does require a bit of a nuanced approach. Let’s walk through the algorithm together:
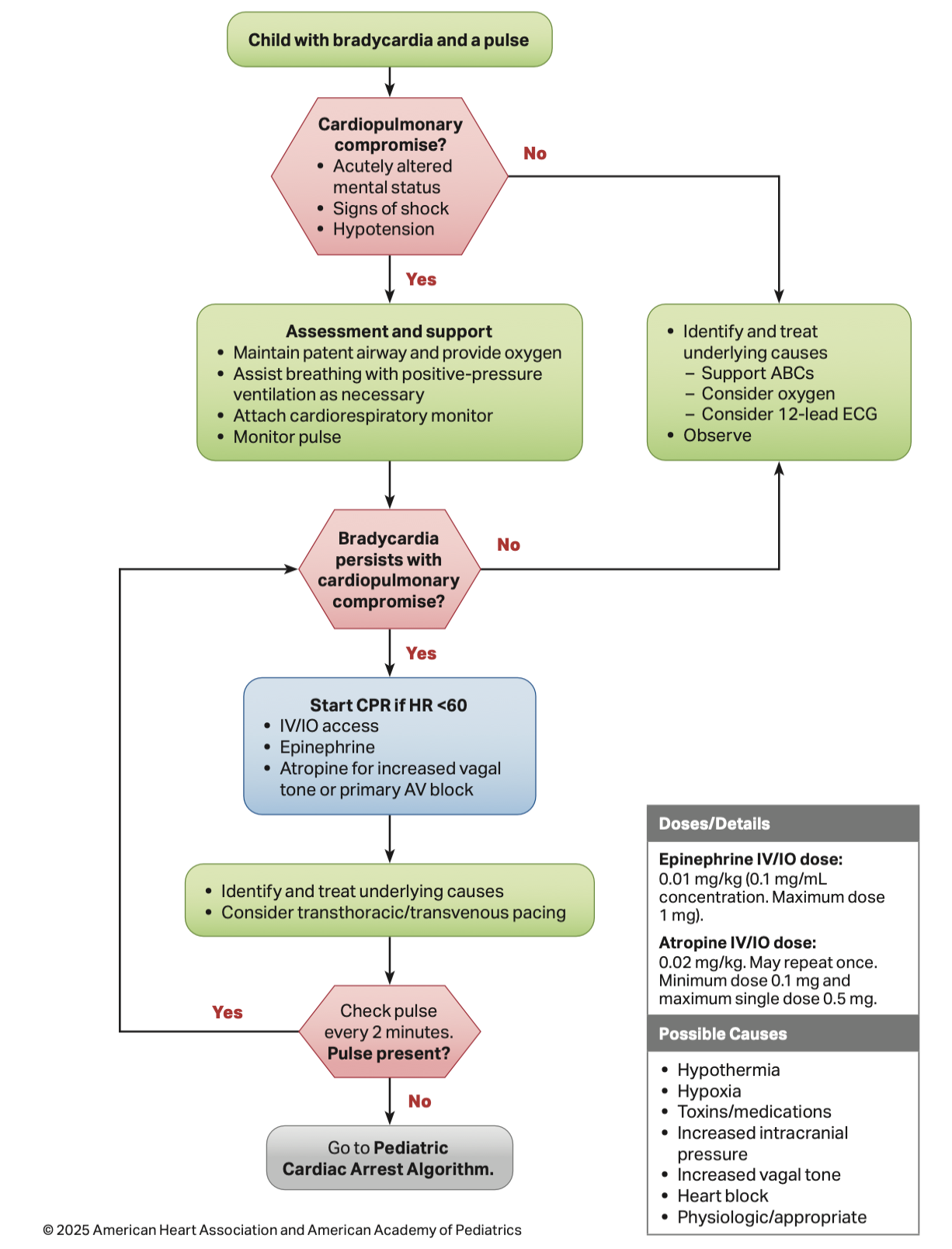
If we find ourselves with a patient exhibiting bradycardia and a pulse, we need to first identify if there is cardiopulmonary collapse, defined as acutely altered mental status, signs of shock, or hypotension. If none of these are present, the algorithm suggests that we identify and treat the underlying causes, support the ABCs, consider O2, consider a 12-lead ECG, and observe. In cases where CPR is not yet indicated, rapid transport to definitive care should be considered early.
If there are signs of cardiopulmonary collapse, we should maintain a patent airway, provide O2, and assist breathing with PPV as necessary.
If the bradycardia persists with cardiopulmonary compromise, it is at this stage that we should start CPR if HR<60, reassessing every 2 minutes.
Importantly however, not all children with bradycardia, even if there are signs of hypoperfusion such as delayed cap refill or mottling, will have impaired LOA. Thus we generally recommend reserving CPR administration to the patients that are severely altered/ unconscious. CPR can be withheld if perfusion is adequate enough that the child is visibly uncomfortable during chest compressions. In this case, focus turns back to adequate oxygenation and standard shock care in this case.
The approach of first providing oxygenation and ventilation through airway repositioning and breath administration is also recommended within the pediatric Basic Life Support Algorithm as well.
For your reference, we have attached those two algorithms.
In summary, while it is appropriate to initiate CPR in a pediatric patient who has a HR<60, this should only occur in the presence of poor perfusion despite oxygenation and ventilation.
References
2025 AHA Guidelines
BLS PCS
ALS PCS
